Picture this: you’ve finally made it to retirement. The kids are grown, the alarm clock is collecting dust, and your calendar is filled with brunches, not board meetings. Life should feel like one long exhale. But then—bam!—you hit the pharmacy, and suddenly your golden years come with a gold-plated price tag. One prescription here, one refill there, and before you know it, your monthly meds are draining your savings faster than you can say “Part D donut hole.”
It’s not just annoying—it’s outrageous. Some of the most common prescriptions retirees rely on are also some of the worst offenders when it comes to cost. And no, it’s not just you—these meds are wildly overpriced across the board. So if you’re tired of choosing between blood pressure pills and the beach vacation you’ve been planning since 1987, this list is for you. Let’s break down the top 13 meds quietly sabotaging your retirement budget—and what to watch out for before your next refill.
1. Ozempic: The Glamorous Glucose Gobbler

If you’ve been hearing about Ozempic non-stop lately, you’re not alone—it’s the celeb-endorsed injectable that’s become a cultural phenomenon. But beneath all the hype lies a price tag that’s straight-up outrageous for most retirees: over $1,000 a month if you’re paying cash. According to Healthline, even with Medicare, copays vary wildly, and it’s not always covered consistently depending on your diagnosis. Some plans cover it for type 2 diabetes but not for weight management, which creates a weird insurance gray zone.
The high demand (thanks to TikTok and Hollywood buzz) has created supply issues, too—so even if you can afford it, you might not find it. For retirees who need it for diabetes, this turns managing your condition into a high-stakes game of pharmacy roulette. And if you’re taking it off-label for weight loss? Forget about insurance covering a dime. This is a drug that works, but it works best when it doesn’t wreck your savings. Before you commit to the hype, talk to your doc about your goals and what you can realistically afford long term. Because being healthy doesn’t mean taking out a loan to keep your blood sugar in check.
2. Januvia: Diabetes Control That Comes With Sticker Shock

Managing type 2 diabetes is already a full-time job, and Januvia adds a full-time cost. It’s a once-a-day pill that helps regulate blood sugar, but at over $500 a month without coverage, it’s a serious threat to your checking account. Even with Medicare, the copays can land somewhere between “annoying” and “are you serious?”
Per AJMC, Januvia is one of the top 10 drugs by spending under Medicare Part D, and seniors are feeling the squeeze. It’s especially frustrating because unlike insulin, there aren’t as many affordable generic alternatives yet. Some people are switching to older diabetes drugs or combining cheaper meds just to avoid hitting the dreaded coverage gap (aka the “donut hole”). And let’s be honest—medical decisions should be about health, not price tags. Talk to your provider or pharmacist about manufacturer savings cards, or see if your plan offers tiered options. No one should have to skip a necessary med just to make rent. Or you know, buy groceries.
3. Revlimid: Cancer Treatment With a Cruel Price
Revlimid is used to treat multiple myeloma, and it’s one of those meds that can quite literally save lives—but also financially destroy them. A single month’s supply can cost over $10,000 without insurance. Even with Medicare, patients can still be stuck with several thousand in annual out-of-pocket costs.
A deep dive by ProPublica found that prices have continued to climb year after year, even though the medication itself hasn’t changed. The company behind it has raised the price more than 20 times since launch, and generic competition is barely trickling in. This makes it one of the most devastating drugs financially for seniors battling cancer. Some patients are forced to go into medical debt, crowdfund, or even skip doses. That’s not just unfair—it’s cruel. The emotional toll of cancer is already unbearable. Add financial strain on top of that? It’s criminal. If you or a loved one takes Revlimid, demand that your oncology team walk you through all available assistance programs, nonprofits, and clinical trial options. Every dollar saved counts.
4. Humira: Arthritis Relief at a Retirement-Ending Cost

Humira has been the poster child for overpriced medication for years—and it’s still cashing in. Prescribed for everything from rheumatoid arthritis to Crohn’s disease, it’s injected every couple of weeks and costs a jaw-dropping $6,000+ a month without insurance. Even Medicare enrollees can pay thousands each year, depending on their plan and usage.
AJMC reported that even though Humira finally has some biosimilar competitors, the price war hasn’t helped patients much yet. That’s because pharmacy benefit managers and drug manufacturers play a weird rebate game that keeps the original drug on top. So instead of prices dropping like we’d all hoped, patients are still paying through the nose (and elbow and spine). If you’re on Humira, it’s time to get nosy about biosimilars. Ask your doctor if you qualify for any of the new alternatives or if they’re covered on your plan. Because honestly, arthritis is painful enough—you shouldn’t need a financial ice pack too.
5. Eliquis: The Blood Thinner Bleeding Your Wallet Dry
Eliquis is a big deal for people with atrial fibrillation or blood clot risks—but the price tag is no joke. A 30-day supply can run upwards of $600 without insurance, and even Medicare users often end up paying hundreds in copays. It’s the kind of cost that turns “life-saving” into “budget-wrecking.”
According to KFF.org, Eliquis is one of the top drugs by total Medicare spending, racking up billions each year. That’s not just a few folks—it’s a systemic hit to retiree wallets nationwide. Despite being on the market for years, there’s no generic version in the U.S. yet because of ongoing patent protection. Which means the brand name keeps its monopoly—and the price stays sky high. If you’re on Eliquis, ask your doc if there’s any wiggle room for alternatives, discounts, or patient assistance programs. And definitely double-check your Part D plan, because the coverage differences can be wild. Otherwise, it’s hard not to feel like your heart medication is giving your budget heart palpitations.
6. Xarelto: The Other Expensive Blood Thinner

You’d think we could get a group discount on blood thinners by now, but no—Xarelto is right up there with Eliquis in the price-gouging Olympics. It’s prescribed for everything from DVT to stroke prevention, and it’s incredibly common among retirees. But each monthly refill can cost over $500 without insurance, and with Medicare Part D, the copay isn’t always much friendlier.
According to AJMC, Xarelto ranks among the highest-spending drugs under Medicare, costing billions in taxpayer dollars and retiree out-of-pocket fees. What’s wild is that it’s not a new drug, and still—no generic available in the U.S. yet. Many seniors find themselves choosing between this and its rival (Eliquis), hoping one plan offers a better deal. But that’s like picking between two equally expensive bottles of wine when you just want something to keep your heart beating. If your doctor suggests it, ask about financial aid programs directly from the manufacturer or if there are discounts available at specific pharmacies. Your bloodstream might be flowing smoothly—but your savings account? Not so much.
7. Trulicity: Weekly Shots, Monthly Sticker Shock

Trulicity’s whole vibe is “set it and forget it”—a once-a-week injection for type 2 diabetes that promises stable blood sugar without the daily hassle. But don’t let the convenience fool you: this drug’s price tag can punch a $900 hole in your wallet every single month without coverage. Even with Medicare, the cost can hit $200–$400 depending on your plan. And if you’re on a fixed income? That’s the weekly grocery budget…gone.
Many retirees feel blindsided after being prescribed it, not realizing how few affordable alternatives exist in the same drug class. Plus, skipping doses to save money completely defeats the purpose—this med works best with consistency. While it is effective for both blood sugar and modest weight loss, it’s a classic case of health vs. wealth. The real kicker? It’s become trendy with younger folks using it off-label for weight loss, driving up demand and keeping prices sky-high. If you’re taking Trulicity, keep an eye out for coupon programs or samples from your provider. And if the cost is breaking you, ask your doctor about less buzzy—but more budget-friendly—options that still work.
8. Entresto: A Heart Failure Med That’s Rough on the Budget
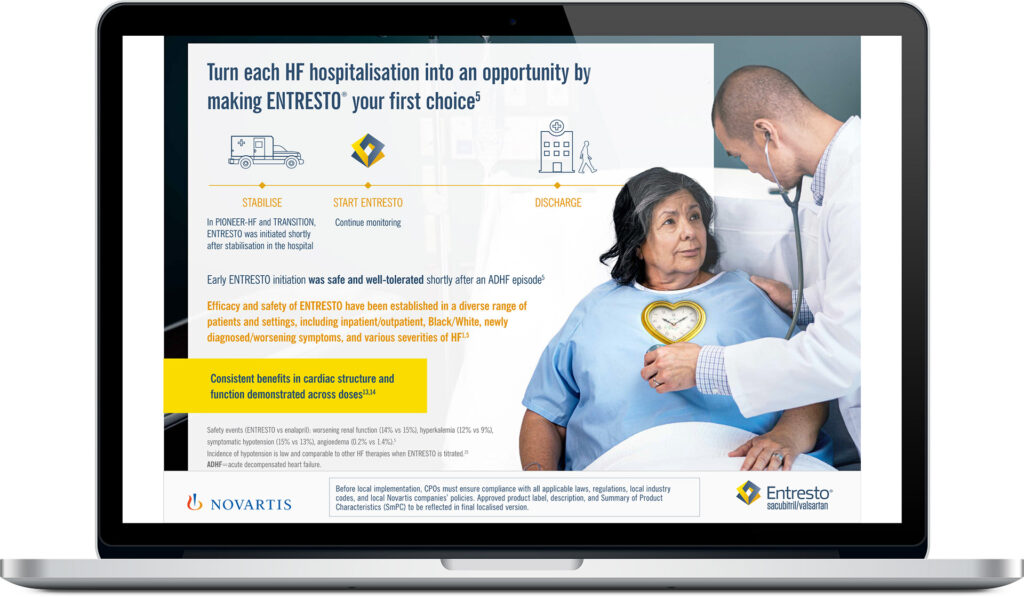
Entresto is a powerhouse when it comes to treating heart failure, improving both quality of life and survival rates. But it comes at a cost that makes your actual heart skip a beat—often around $600 per month without insurance. Even with Medicare, many seniors end up in the dreaded “donut hole,” where out-of-pocket costs spiral out of control. That means your life-saving medication might force you to cut back on, well…everything else.
And that’s the cruel irony: stay alive, but maybe skip eating out, traveling, or enjoying retirement. Some patients don’t even know there are alternative medications that are older, cheaper, and still effective. The pharma hype machine tends to drown out those conversations. Entresto also requires routine bloodwork, which adds to the overall expense. While it may absolutely be the right med for you, it shouldn’t come at the price of constant financial anxiety. Make sure your cardiologist actually discusses cost with you—don’t be shy about bringing it up. Because if your heart meds are giving you money-related stress, that kind of defeats the whole point, right?
9. Advair Diskus: Breathing Relief That’s Gasp-Inducing at the Pharmacy

For anyone with asthma or COPD, Advair Diskus can be a literal lifesaver. It helps keep your lungs open and your flare-ups in check—but the cost can take your breath away. Without insurance, it’s around $400 a month, and even with coverage, some folks pay $100 or more per refill. Inhalers, in general, are notoriously expensive in the U.S., and this one’s no exception.
Worse, many people don’t use it daily as prescribed because they’re trying to stretch it longer, which ends up making things worse. The result? Emergency room visits that cost way more than just filling the prescription. If you’re dependent on Advair, make sure your pharmacist checks for lower-cost generics or similar meds. Some plans may cover Symbicort or Breo instead—worth asking! Also, check manufacturer coupons or pharmacy discount cards, which can sometimes slash the price by 50% or more. You deserve to breathe easy without having a panic attack at the register.
10. Lyrica: Nerve Pain Relief That Hurts Your Bank Account

Lyrica is often prescribed for nerve pain, fibromyalgia, or even seizures—but the financial pain it causes is very real. A month’s supply can cost up to $700 without insurance, and with Medicare, you’re still looking at some steep copays. For people dealing with chronic pain, skipping it isn’t an option—but affording it? That’s a whole different battle.
Some people try to cut pills in half or take them less frequently, but that often leads to flare-ups or reduced effectiveness. Even when a generic version (pregabalin) is available, it’s not that much cheaper depending on your plan. The real tragedy? There are often cheaper alternatives out there, but they might not be suggested right away unless you press for them. This is one of those drugs where a little shopping around can make a big difference. Try GoodRx or your local pharmacy’s discount club. Also, ask about non-drug therapies that may supplement or reduce your need for high doses. Chronic pain sucks—but your finances shouldn’t suffer, too.
11. Imbruvica: Cancer Care That Comes With a Luxury Price Tag

If you’re taking Imbruvica, chances are you’re dealing with something major like chronic lymphocytic leukemia or lymphoma. It’s a targeted therapy that can slow disease progression and even extend life—but it’s also priced like a private jet charter. A month’s supply costs over $14,000 without insurance. Yes, you read that right.
Even with Medicare Part D, patients can pay thousands out-of-pocket each year, especially once they hit catastrophic coverage levels. And unfortunately, skipping doses or rationing to save money can reduce effectiveness and speed up disease progression. It’s one of the harshest examples of how prescription drug pricing can push even the most stable retiree into financial panic. If you’re on Imbruvica, ask your oncology team immediately about assistance programs from the manufacturer. There are also cancer-specific nonprofits that can help offset the cost. And don’t be afraid to bring in a financial navigator or case manager—most cancer centers have one. Cancer treatment is already an emotional and physical marathon—there’s no reason it should bankrupt you, too.
12. Restasis: Dry Eye Drops That’ll Make You Cry

Restasis is the go-to prescription for chronic dry eye—aka that burning, gritty feeling that never seems to quit. And while a little eye relief might sound minor, the cost is anything but. A month’s supply can set you back over $600 without coverage. Even with Medicare, copays are surprisingly high for something that comes in such a tiny bottle.
It doesn’t help that Restasis is often prescribed as a long-term treatment, not a one-time fix. That means month after month of shelling out cash just to stop feeling like you’re blinking over sandpaper. Some people have turned to over-the-counter alternatives, but they’re usually less effective. If you’re struggling with cost, ask your eye doctor about generic cyclosporine, which may offer relief for less. Also, some dry eye sufferers benefit from humidifiers, warm compresses, or lifestyle tweaks that can reduce dependence on drops. Your eyes deserve relief, sure—but not at the cost of your vacation fund.
13. Abilify: Mental Health Maintenance That’s Financially Draining

Abilify is prescribed for everything from depression and bipolar disorder to schizophrenia, and it’s a staple in many retirees’ medicine cabinets. But it’s also notorious for its hefty price tag—around $800 a month without insurance. Even Medicare enrollees can face sizable costs depending on their plan tier. That’s a lot of money to stay balanced.
And let’s be clear: stopping or reducing your dose without guidance can seriously mess with your mental health. This is a med that needs consistency, which makes its high cost extra risky. The good news? A generic version (aripiprazole) is available and can be much cheaper—if your doctor and plan are on the same page. Some folks don’t even realize they’re paying full freight when there’s a generic option just a conversation away. Mental health meds should never be out of reach. If the cost is causing more stress than the condition itself, it’s time to revisit your plan, your pharmacy, or your provider’s willingness to advocate for you. Sanity should be covered—period.
This article is for informational purposes only and should not be construed as financial advice. Consult a financial professional before making investment or other financial decisions. The author and publisher make no warranties of any kind.